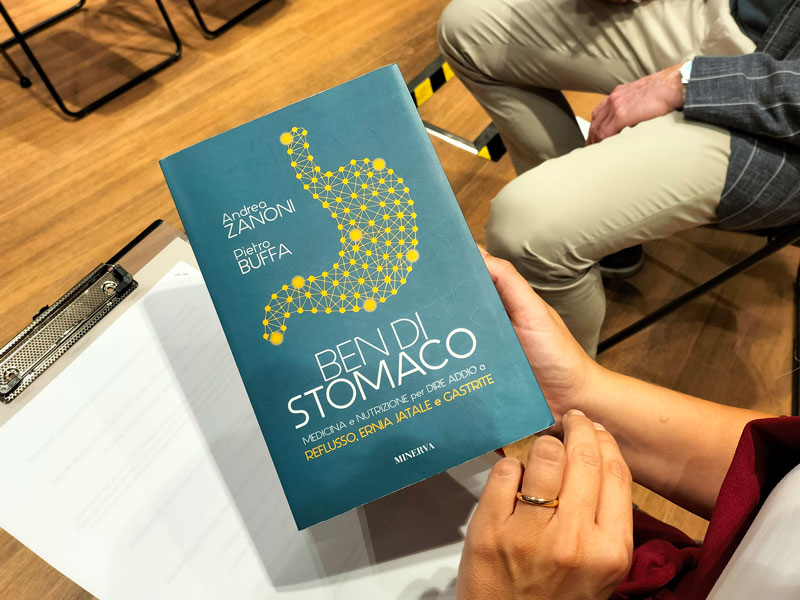
Ben di stomaco
Medicina e nutrizione per dire addio a REFLUSSO, ERNIA JATALE e GASTRITE








Almeno 1 persona su 5 soffre di problemi di stomaco.
Un uso combinato e sapiente di medicina e nutrizione può aiutare a trovare una soluzione efficace e duratura. Questo testo semplice, ma non banale, vi permetterà di dire addio a reflusso e bruciore di stomaco.
Lo stomaco è senz’altro un organo che dobbiamo tenere in perfetta efficienza e molti aspetti della nutrizione rivestono oggi un ruolo fondamentale per rimettere in salute quest’organo e attraverso esso, tutto il nostro organismo. Bruciore di stomaco, gastrite, peso allo stomaco, ma anche semplicemente mal di pancia: una persona si riferisce ai disturbi di stomaco ed esofago in molti modi diversi. Il mal di stomaco infatti è diffusissimo, in tutte le sue forme, dalla gastrite al reflusso: si stima ad esempio che nei Paesi occidentali tra il 10 ed il 20% della popolazione soffra di reflusso.
Visita il mio profilo

Adenocarcinoma della giunzione esofago-gastrica

E’ una grande soddisfazione vedere il nostro libro “Adenocarcinoma of the esophagogastric junction” tradotto in cinese.
RAI 2 – Eat Parade TG” – 23.12.22
Non tutti hanno problemi di stomaco, ma è molto probabile che abbiamo parenti o amici cui potrebbe essere d’aiuto avere informazioni in più su questo genere di disturbo!
La maggior parte dei pazienti è affetta da forme lievi, che necessitano di sola terapia medica episodica. Tuttavia, una significativa fetta di pazienti richiede terapie a lungo termine, che possono includere anche l’opzione chirurgica. Il linguaggio medico purtroppo non aiuta, crea barriere, spesso è comprensibile solo tra addetti ai lavori e il paziente lo segue con difficoltà.
Un medico-chirurgo esperto in malattie gastro-esofagee (Andrea Zanoni) e un biologo molecolare e nutrizionista (Pietro Buffa), offrono ai non addetti ai lavori una spiegazione chiara e non banale su cosa sia e come si curi il mal di stomaco.
Due figure professionali, che si occupano quotidianamente della salute dello stomaco e della risoluzione delle eventuali problematiche ad esso associate, hanno deciso di raccontare in modo piacevole, con esempi ed episodi di storia della medicina, come funzionino gli eventuali esami diagnostici e le terapie mediche e cosa succeda in sala operatoria, per chi avesse la necessità di sottoporsi ad un intervento chirurgico, evidenziando anche che la corretta nutrizione è indispensabile per il nostro benessere.
Disturbi di stomaco: cause, terapie e soluzioni
«In medicina il punto cruciale non è solo la comunicazione tra colleghi, bensì anche e soprattutto quella tra medico e paziente – afferma Andrea Zanoni –. Questo è il tema del nostro libro: far capire al paziente in modo semplice, cosa siano queste malattie diffuse, fortunatamente spesso non gravi, tuttavia molto invalidanti. Mi occupo di reflusso perche ritengo che una materia complessa come questa meriti specialisti dedicati, per evitare il pericoloso “fai da te” utilizzando il “dottor Google”, che può portare a grossi danni. Scrivo questo libro perché i pazienti meritano si spieghi loro che cosa sia il reflusso in maniera comprensibile.»
«Collaborazioni come queste – spiega Pietro Buffa – in cui gli aspetti nutrizionali sono complementari alla medicina classica convenzionale, risultano vincenti e andrebbero certamente applicati a molti più ambiti della salute pubblica. La nutrizione rappresenta una parte sostanziale di quella che oggi viene definita Medicina Integrata, un tipo di medicina che si pone l’obbiettivo di “integrare” l’approccio medico convenzionale con tecniche e discipline di supporto volte al benessere dell’individuo nella sua globalità, partendo da un semplice ma chiaro insegnamento che, già nel 400 a.C., il medico greco Ippocrate ci lasciava in eredità: “Fa che il cibo sia la tua medicina e la medicina il tuo cibo”.»

“Un’emozione nella mia vita è una cena senza bruciori di stomaco.”
Woody Allen
Parlano di Ben di Stomaco
TeleArena – 23 Settembre 2022
Odeon TV – 18 Settembre 2022
Intervista 9MQ – Giugno 2022

Starbene Dicembre 2022



Giornale F – Settembre 2022




Alcune pubblicazioni
Adenocarcinoma of the esophagogastric junction
PubMed - VEDI IL LINK
Value of routine timed barium esophagram follow-up in achalasia after myotomy.
PubMed - VEDI IL LINK
Value of routine timed barium esophagram follow-up in achalasia after myotomy.
Kachala SS, Rice TW, Baker ME, Rajeswaran J, Thota PN, Murthy SC, Blackstone EH, Zanoni A, Raja S.
J Thorac Cardiovasc Surg. 2018 Mar 8. pii: S0022-5223(18)30621-4. doi: 10.1016/j.jtcvs.2018.03.001
Abstract
OBJECTIVES: The value of routine timed barium esophagram (TBE) in longitudinal follow-up of achalasia after Heller myotomy is unknown. We prospectively prescribed a yearly follow-up TBE. Purposes were to characterize esophageal emptying over time after myotomy, identify preoperative TBE measures associated with follow-up TBE, and characterize follow-up TBE over time in relationship to reintervention.
METHODS: From March 1995 to April 2013, 635 patients underwent Heller myotomy for achalasia; 559 had at least 1 follow-up TBE. Temporal trends of 1335 follow-up TBEs in all nonreintervention and reintervention patients were assessed. Multivariable longitudinal analysis identified preoperative TBE measures associated with follow-up TBE.
RESULTS: On average, TBE height and width at 1 and 5 minutes decreased approximately 50% and 60%, respectively, at first postoperative follow-up, and remained stable or slightly decreased for up to 5 years. Wider TBE width at 5 minutes was associated with greater follow-up TBE height and width at 1 minute. Of 118 patients undergoing reintervention, 64 (57%) had only 1 reintervention, with follow-up TBE returning to that of nonreintervention patients. Patients whose follow-up TBE remained abnormal underwent a further reintervention, some normalizing on subsequent TBE, and some not.
CONCLUSIONS: Follow-up TBE is valuable postmyotomy, particularly if there is substantial esophageal dilatation preoperatively. Follow-up TBE reassures patients with stable or decreasing TBE measures, permitting decreased follow-up intensity. Reintervention should not be considered a myotomy failure, because a successful, single, nonsurgical reintervention often results in long-term successful palliation. More than 1 reintervention requires intensification of TBE follow-up, facilitating treatment planning.
Adenocarcinoma: treatment update.
PubMed - VEDI IL LINK
Siewert III adenocarcinoma: treatment update.
Di Leo A, Zanoni A.
Updates Surg. 2017 Sep;69(3):319-325. doi: 10.1007/s13304-017-0429-9.
Abstract
Siewert III cancer, although representing around 40% of EGJ cancers and being the EGJ cancer with worst prognosis, does not have a homogenous treatment, has few dedicated studies, and is often not considered in study protocols. Although staged as an esophageal cancer by the TNM 7th ed., it is considered a gastric cancer by new TNM 8th ed. Our aim was to consolidate the current literature on the indications and treatment options for Siewert III adenocarcinoma. A review of the literature was performed to better delineate treatment indications (according to stage, surgical margins, type of lymphatic spread and lymphadenectomy) and treatment strategy. The treatment approach is strictly dependent on cancer site and nodal diffusion. T1m cancers have insignificant risk of nodal metastases and can be safely treated with endoscopic resections. The risk of nodal metastases increases markedly starting from T1sm cancers and requires surgery with lymphadenectomy. The site of this type of cancer and the nodal diffusion require a total gastrectomy and distal esophagectomy, with 5 cm of clear proximal and distal margins and a D2 abdominal and inferior mediastinal lymphadenectomy. Multimodal treatments are indicated in all locally advanced and node positive cancers. Siewert III cancers are gastric cancers with some peculiarities and require dedicated studies and deserve more consideration in the current literature, especially because their treatment is particularly challenging
Nodal downstaging in esophageal and esophagogastric junction cancer: more important than ever.
PubMed - VEDI IL LINK
ARTICOLO COMPLETO
Nodal downstaging in esophageal and esophagogastric junction cancer: more important than ever.
Zanoni A.
J Thorac Dis. 2017 Jul;9(7):1839-1842. doi: 10.21037/jtd.2017.06.126.
Comment on: Prognostic Value of Pretreatment Pathological Tumor Extent in Patients Treated With Neoadjuvant Chemoradiotherapy Plus Surgery for Esophageal or Junctional Cancer. [Ann Surg. 2017]
Radical surgery for gastric cancer in octogenarian patients.
PubMed - https://pubmed.ncbi.nlm.nih.gov/28493221/
Casella F, Sansonetti A, Zanoni A, Vincenza C, Capodacqua A, Verzaro R.
Updates Surg. 2017 Sep;69(3):389-395. doi: 10.1007/s13304-017-0463-7.
Abstract
To valuate feasibility and results of radical surgery in octogenarian patients with gastric cancer. We collected data on 60 patients that underwent gastrectomy with an R0 resection at our Institution from 2010 to 2015. Patients were divided into two groups: octogenarian (OG) (n = 26), consisting of patients aged 80-89 years, and younger (YG) (n = 34), consisting of patients under 80 years of age. All patients were treated with total or subtotal gastrectomy with lymphadenectomy. A D2-lymphadenectomy was performed in 11 and 24 patients, a D1+ in 5 and 4, a D1 in 8 and 6, and a D0 in 2 and 0 cases in OG and YG respectively. The overall morbidity rate was 42.3% (11/26) in OG and 29.4% (10/34) in YG, while 90-days mortality was observed in four (15.4%) and one (2.9%) patients in OG and YG, respectively. The median hospital stay was 9 days (2-31) and 9.5 days (6-66) in OG and YG, respectively. Gastrectomy with radical resection and limited lymphadenectomy should be recommended for octogenarian patients with good performance status and low co-morbidity.
Genetic prediction of long-term survival after neoadjuvant chemoradiation in locally advanced esophageal cancer.
PubMed - VEDI IL LINK
Gusella M, Giacopuzzi S, Bertolaso L, Zanoni A, Pezzolo E, Modena Y, Menon D, Paganin P, Weindelmayer J, Crepaldi G, De Manzoni G, Pasini F.
Pharmacogenomics J. 2017 Jun;17(3):252-257. doi: 10.1038/tpj.2016.9.
Abstract
Candidate genes involved in DNA repair, 5-fluorouracil metabolism and drug detoxification were genotyped in 124 patients receiving neoadjuvant chemoradiation treatment for locally advanced esophageal cancer and their predictive role for long-term relapse-free survival (RFS) and cancer-specific survival (CSS) were evaluated. A panel including MTHFR 677TT, MDR1 2677GT, GSTP1 114CC, XPC 499CC and XPC 939AC+CC, defined as high-risk genotypes, discriminated subgroups with significantly different outcomes. When the panel was combined with histology, patients split into two subsets with 5-year RFS and CSS rates of 65% vs 27% (hazard ratio (HR) 3.0, P<0.0001) and 69% vs 31% (HR 2.9, P<0.0001), respectively. Combining the 5-single-nucleotide polymorphism (5-SNP) panel with pathological response defined two major informative risk classes with 5-year PFS and CSS rates of 79.4% vs 17.7% (HR 6.71, P<0.0001) and 79.3% vs 26.3% (HR 6.25, P<0.0001), respectively. This classification achieved a sensitivity of 79%, a specificity of 85.4% and an accuracy of 81.8%.
Extended lymphadenectomy in elderly and/or highly co-morbid gastric cancer patients: A retrospective multicenter study.
PubMed - VEDI IL LINK
Rausei S, Ruspi L, Rosa F, Morgagni P, Marrelli D, Cossu A, Cananzi FC, Lomonaco R, Coniglio A, Biondi A, Cipollari C, Graziosi L, Fumagalli U, Casella F, Bertoli P, di Leo A, Alfieri S, Vittimberga G, Roviello F, Orsenigo E, Quagliuolo V, Montemurro S, Baiocchi G, Persiani R, Bencivenga M, Donini A, Rosati R, Sansonetti A, Ansaloni L, Zanoni A, Galli F, Dionigi G; Italian Research Group for Gastric Cancer (IRGGC).
Eur J Surg Oncol. 2016 Dec;42(12):1881-1889. doi: 10.1016/j.ejso.2016.05.003.
Abstract
BACKGROUND: Gastrectomy with extended lymphadenectomy is considered the gold standard treatment for advanced gastric cancer, with no age- or comorbidity-related limitations. We evaluated the safety and efficacy of curative gastrectomy with extended nodal dissection, verifying survival in elderly and highly co-morbid patients.
METHODS: In a retrospective multicenter study, we examined 1322 non-metastatic gastric-cancer patients that underwent curative gastrectomy with D2 versus D1 lymphadenectomy from January 2000 to December 2009. Postoperative complications, overall survival (OS), and disease-specific survival (DSS) according to age and the Charlson Comorbidity Score were analyzed in relation to the extent of lymphadenectomy.
RESULTS: Postoperative morbidity was 30.4%. Complications were more frequent in highly co-morbid elderly patients, and, although general morbidity rates after D2 and D1 lymphadenectomy were similar (29.9% and 33.2%, respectively), they increased following D2 in highly co-morbid elderly patients (39.6%). D2-lymphadenectomy significantly improved 5-year OS and DSS (48.0% vs. 37.6% in D1, p < 0.001 and 72.6% vs. 58.1% in D1, p < 0.001, respectively) in all patients. In elderly patients, this benefit was present only in 5-year DSS. D2 nodal dissection induced better 5-year OS and DSS rates in elderly patients with positive nodes (29.7% vs. 21.2% in D1, p = 0.008 and 47.5% vs. 30.6% in D1, p = 0.001, respectively), although it was present only in DSS when highly co-morbid elderly patients were considered.
CONCLUSION: Extended lymphadenectomy confirmed better survival rates in gastric cancer patients. Due to high postoperative complication rate and no significant improvement of the OS, D1 lymphadenectomy should be considered in elderly and/or highly co-morbid gastric cancer patients.
ypN0: Does It Matter How You Get There? Nodal Downstaging in Esophageal Cancer.
Zanoni A, Verlato G, Giacopuzzi S, Motton M, Casella F, Weindelmayer J, Ambrosi E, Di Leo A, Vassiliadis A, Ricci F Rice TW, de Manzoni G.
Ann Surg Oncol. 2016 Dec;23(Suppl 5):998-1004.
Abstract
BACKGROUND: pN0 following induction treatment for advanced esophageal cancer improves survival. Importance of how ypN0 is achieved is unknown. This study evaluates survival in “natural” N0 (cN0/ypN0) and “downstaged” N0 (cN+/ypN0) patients.
METHODS: Among patients treated with induction treatment and surgery, 83 CT scans were retrieved in digital format and re-evaluated by a radiologist, blinded to pathological nodal status: 28 natural N0, 37 downstaged N0, and 18 ypN+. Impact of N0 classification on survival and associations with survival were identified.
RESULTS: Survival varied with ypN: 3-year survival was 84 % for natural N0 patients, 59 % for downstaged N0, and 20 % for ypN+ (p < .001). Compared with natural N0 patients, risk of cancer mortality was 3.8 for downstaged N0 and 7.6 for ypN+ (p = .01). Survival was also stratified by ypT: compared with ypT0 natural N0, who had the best survival, intermediate survival was seen in ypT+ natural N0 [hazard ratio (HR), 1.3] and ypT0 downstaged N0 (HR, 1.8), and poor survival in ypT+ downstaged N0 (HR, 9.5) and ypN+ (HR, 12.0) (p = .026).
CONCLUSIONS: Natural N0 and downstaged N0 patients are different clinical entities: downstaging cN+ with induction treatment producing downstaged N0 improves survival only if there is concomitant primary cancer downstaging to ypT0. Intermediate survival is seen in downstaged N0 patients with complete tumor response. Natural N0 patients experience intermediate survival with incomplete response (ypT+). Complete response in natural N0 patients produces the best survival. Means of obtaining ypN0 status matters and requires a complete response for downstaged N0 patients to benefit from induction treatment.
Timed barium esophagram in achalasia types.
PubMed - VEDI IL LINK
Zanoni A, Rice TW, Lopez R, Birgisson S, Shay SS, Thota PN, Baker ME, Raymond DP, Blackstone EH.
Dis Esophagus. 2015 May-Jun;28(4):336-44. doi: 10.1111/dote.12212.
Abstract
Relationships of timed barium esophagram (TBE) findings to achalasia types defined by high-resolution manometry (HRM) have not been elucidated. Therefore, we correlated preoperative TBE and HRM measurements in achalasia types and related these to patient symptoms and prior treatments. From 2006 to 2013, 248 achalasia patients underwent TBE and HRM before Heller myotomy. TBE height and width were recorded at 1 and 5 minutes; HRM measured lower esophageal sphincter mean basal pressure, integrated relaxation pressure (IRP), and mean esophageal body contraction amplitude. Achalasia was classified into types I (25%), II (65%), and III (9.7%). TBE height at 5 minutes was higher for I (median 8 cm; interquartile range 6-12) and II (8 cm; 8-11) than for III (1 cm; 0-7). TBE width at 5 minutes was widest (3 cm; 2-4), narrower in II (2 cm; 2-3), and narrowest in I (1 cm; 0-2), P < 0.001. Volume remaining at 1 and 5 minutes was lower in III (1 m(2) ; 0-16) than I (42 m(2) ; 17-106) and II (39 m(2) ; 15-60), highlighting poorer emptying of I and II. Increasing TBE width correlated with deteriorating morphology and function from III to II to I. Symptoms poorly correlated with TBE and HRM. Prior treatment was associated with less regurgitation, faster emptying, and lower IRP. Although TBE and HRM are correlated in many respects, the wide range of their measurements observed in this study reveals a spectrum of morphology and dysfunction in achalasia that is best characterized by the combination of these studies.
Siewert III esophagogastric junction adenocarcinoma: does TNM 8thsave us?
Zanoni A, Verlato G, Baiocchi GL, Casella F, Cossu A, d’Ignazio A, De Pascale S, Giacopuzzi S.
Updates Surg. 2018 May 28. doi: 10.1007/s13304-018-0537-1. [Epub ahead of print]
Abstract
Siewert III cancers were classified as esophageal cancers by the TNM 7th edition (TNM7), while being defined as gastric cancers by the new TNM 8th edition (TNM8). Aim of this study was to compare previous and present TNM classifications of Siewert III. From 2000 to 2015, 309 patients with Siewert III adenocarcinoma were treated at ten high-volume centers, belonging to the GIRCG (Italian Research Group for Gastric Cancer). We retrospectively analyzed overall survival according to TNM classifications: gastric TNM8 was compared with either gastric TNM7 or esophageal TNM7. Median number of lymph nodes harvested was 31 (interquartile range 22-44). Agreement between gastric TNM7 and TNM8 was very good (weighted kappa 92.3%, IC 95% 90.3-94.1%). Accordingly, stage migration was observed in 54 of 309 patients (17.5%), with 12 patients upstaged (3.9%) and 42 downstaged (13.6%). Cox models including either gastric TNM7 or TNM8 achieved similar goodness-of-fit and c-index. Differences were much larger, when shifting from esophageal TNM7 to gastric TNM8: the agreement was much lower (weighted kappa 69.1%, 65.2-73.2%), with 196 of 309 patients (63.4%) downstaging. The corresponding Cox model presented the lowest goodness-of-fit and discrimination ability. Gastric TNM7 and TNM8 were largely superimposable, so that stage migration was minor and prognostic significance was similar. At variance, stage migration was substantial when shifting from esophageal TNM7 to TNM8. Moreover, survival models with esophageal TNM7 presented the worst goodness-of-fit and the lowest discrimination ability. This further supports placing Siewert III among gastric cancers, as done in TNM8.
Treatment of Esophageal and Hypopharingeal Squamous Cell Carcinoma
Book - VEDI IL LINK
Homogenous approach to esophageal cancer treatment, which is the result of author’s lifetime experience
Exhaustive recent literature review
In each chapter, appropriate tools for correct management of this difficult disease
TAK1-regulated expression of BIRC3 predicts resistance to preoperative chemoradiotherapy in oesophageal adenocarcinoma patients.
PubMed - VEDI IL LINK
ARTICOLO COMPLETO
Piro G, Giacopuzzi S, Bencivenga M, Carbone C, Verlato G, Frizziero M, Zanotto M, Mina MM, Merz V, Santoro R, Zanoni A, De Manzoni G, Tortora G, Melisi D.
Br J Cancer. 2015 Sep 15;113(6):878-85. doi: 10.1038/bjc.2015.283.
Abstract
BACKGROUND: About 20% of resectable oesophageal carcinoma is resistant to preoperative chemoradiotherapy. Here we hypothesised that the expression of the antiapoptotic gene Baculoviral inhibitor of apoptosis repeat containing (BIRC)3 induced by the transforming growth factor β activated kinase 1 (TAK1) might be responsible for the resistance to the proapoptotic effect of chemoradiotherapy in oesophageal carcinoma.
METHODS: TAK1 kinase activity was inhibited in FLO-1 and KYAE-1 oesophageal adenocarcinoma cells using (5Z)-7-oxozeaenol. The BIRC3 mRNA expression was measured by qRT-PCR in 65 pretreatment frozen biopsies from patients receiving preoperatively docetaxel, cisplatin, 5-fluorouracil, and concurrent radiotherapy. Receiver operator characteristic (ROC) analyses were performed to determine the performance of BIRC3 expression levels in distinguishing patients with sensitive or resistant carcinoma.
RESULTS: In vitro, (5Z)-7-oxozeaenol significantly reduced BIRC3 expression in FLO-1 and KYAE-1 cells. Exposure to chemotherapeutic agents or radiotherapy plus (5Z)-7-oxozeaenol resulted in a strong synergistic antiapoptotic effect. In patients, median expression of BIRC3 was significantly (P<0.0001) higher in adenocarcinoma than in the more sensitive squamous cell carcinoma subtype. The BIRC3 expression significantly discriminated patients with sensitive or resistant adenocarcinoma (AUC-ROC=0.7773 and 0.8074 by size-based pathological response or Mandard's tumour regression grade classifications, respectively).
CONCLUSIONS: The BIRC3 expression might be a valid biomarker for predicting patients with oesophageal adenocarcinoma that could most likely benefit from preoperative chemoradiotherapy.
Neoadjuvant concurrent chemoradiotherapy for locally advanced esophageal cancer in a single high-volume center.
Zanoni A, Verlato G, Giacopuzzi S, Weindelmayer J, Casella F, Pasini F, Zhao E, de Manzoni G.
Ann Surg Oncol. 2013 Jun;20(6):1993-9. doi: 10.1245/s10434-012-2822-4.
Abstract
BACKGROUND: Neoadjuvant chemoradiotherapy (CRT) is now considered the standard of care by many centers in the treatment of both squamous cell carcinoma (SCC) and adenocarcinoma of the esophagus. This study evaluates the effectiveness of a neoadjuvant CRT protocol, as regards pathological complete response (pCR) rate and long-term survival.
METHODS: From 2003 to 2011, at Upper G.I. Surgery Division of Verona University, 155 consecutive patients with locally advanced esophageal cancers (90 SCC, 65 adenocarcinoma) were treated with a single protocol of neoadjuvant CRT (docetaxel, cisplatin, and 5-fluorouracil with 50.4 Gy of concurrent radiotherapy). Response to CRT was evaluated through percentage of pathological complete response (pCR or ypT0N0), overall (OS) and disease-related survival (DRS), and pattern of relapse.
RESULTS: One hundred thirty-one patients (84.5 %) underwent surgery. Radical resection (R0) was achieved in 123 patients (79.3 %), and pCR in 65 (41.9 %). Postoperative mortality was 0.7 % (one case). Five-year OS and DRS were respectively 43 and 49 % in the entire cohort, 52 and 59 % in R0 cases, and 72 and 81 % in pCR cases. Survival did not significantly differ between SCC and adenocarcinoma, except for pCR cases. Forty-nine patients suffered from relapse, which was mainly systemic in adenocarcinoma. Only three out of 26 pCR patients with previous adenocarcinoma developed relapse, always systemic.
CONCLUSIONS: This study suggests that patients treated with the present protocol achieve good survival and high pCR rate. Further research is necessary to evaluate whether surgery on demand is feasible in selected patients, such as pCR patients with adenocarcinoma.
Neoadjuvant therapy with weekly docetaxel and cisplatin, 5-fluorouracil continuous infusion, and concurrent radiotherapy in patients with locally advanced esophageal cancer produced a high percentage of long-lasting pathological complete response: a phase 2 study.
PubMed - VEDI IL LINK
ARTICOLO COMPLETO
Pasini F, de Manzoni G, Zanoni A, Grandinetti A, Capirci C, Pavarana M, Tomezzoli A, Rubello D, Cordiano C.
Cancer. 2013 Mar 1;119(5):939-45. doi: 10.1002/cncr.27822.
Abstract
BACKGROUND: This phase 2 study was aimed at defining the pathological response rate of a neoadjuvant schedule including weekly docetaxel and cisplatin, continuous infusion (c.i.) of 5-fluorouracil (5-FU) and concomitant radiotherapy (RT) in untreated stage II-III adenocarcinoma and squamous cell carcinoma of mid-distal thoracic esophagus.
METHODS: The schedule consisted of a first phase of chemotherapy alone and of a second phase of concurrent chemoradiation. Doses were as follows: docetaxel 35 mg/m(2) and cisplatin 25 mg/m(2) on days 1, 8, 15, 29, 36, 43, 50, and 57 plus 5-FU c.i. (180 mg/m(2) on days 1-21 and 150 mg/m(2) on days 29-63); RT (50 Gy) started at day 29. Surgery was planned 6 to 8 weeks after the completion of chemoradiation.
RESULTS: A total of 74 patients were enrolled; pathological complete remission (pCR) was found in 47% (35 of 74) and near pCR (microfoci of tumor cells on the primary tumor without lymph nodal metastases) (pnCR) in 15% of the patients (11 of 74). Grade 3-4 neutropenia, nonhematological toxicity, and toxic deaths occurred in 13.5%, 32.4%, and 4% of the patients, respectively. Median follow-up was 55 months (range, 3-108 months). Median survival of all 74 patients was 55 months, whereas it was not reached in the pCR subset. The 3- and 5-year survival rates were, respectively, 83% and 77% for pCR, 73% and 44% for pnCR, and 21% and 14% for Residual Tumor subsets (P < .001).
CONCLUSIONS: This study shows that 1) this intensive weekly schedule produced a high pathological response rate, 2) responders had high and long-term durable survival rates.
Treatment of esophago-gastric junction adenocarcinoma.
PubMed - VEDI IL LINK
de Manzoni G, Zanoni A, Giacopuzzi S.
Ann Ital Chir. 2012 May-Jun;83(3):208-14.
Abstract
AIM: The incidence of Adenocarcinoma of the esophagogastric junction (EGJ) is increasing and its treatment is still debated, primarily because of the non-uniform definition of EGJ.
MATERIALS AND METHODS: The most used classification of EGJ cancer was proposed by Siewert and it divides the EGJ in three regions: from 5 to 1 cm above the Z line (Siewert type I or esophageal Adenocarcinoma), from 1 over to 2 below the Z line (Siewert type II or real Cardia cancer) and from 2 below to 5 below the Z line (Siewert type III or proximal Gastric cancer diffused to Cardia). The neoplasia is defined type I, II or III depending on where is the center of the cancer.
DISCUSSION: This classification did not show to be related to differences in prognosis and survival, but it has been used to guide the surgical strategy based on the site of the tumor. Criticism about this classification focuses mainly on the non-uniform treatment, in the current literature, of Siewert Type II cancer.
CONCLUSION: From January 2010, a new definition of EGJ carcinoma has been introduced by TNM. This new definition considers esophageal cancers all the ones whose centers falls inside a line drawn 5 cm below the Z line with invasion of the esophagus. This means that Siewert type I and II are now considered esophageal cancers, while type III can be esophageal or proximal gastric cancer depending if the esophagus is infiltrated or not. Criticism about this new definition rises on the border-line definition of former Siewert type III cancers.
pat. Lorem ipsum dolor sit amet, consectetur adipiscing elit. Cras ultricies ligula sed magna dictum porta. Nulla porttitor accumsan tincidunt. Sed porttitor lectus nibh. Cras ultricies ligula sed magna dictum porta. Praesent sapien massa, convallis a pellentesque nec, egestas non nisi.
Response to induction therapy in oesophageal and cardia carcinoma using Mandard tumour regression grade or size of residual foci.
PubMed - VEDI IL LINK
Verlato G, Zanoni A, Tomezzoli A, Minicozzi A, Giacopuzzi S, Di Cosmo M, Franceschetti I, de Manzoni G.
Br J Surg. 2010 May;97(5):719-25. doi: 10.1002/bjs.6949.
Abstract
BACKGROUND: Tumour regression grade (TRG) is used to evaluate responses to induction therapy in cancer of the oesophagus or cardia. This study aimed to determine whether inclusion of node category could improve the prognostic accuracy provided by TRG, and explore the prognostic value of an alternative classification based on size of residual foci and node category.
METHODS: Patients with oesophageal or cardia cancer treated with neoadjuvant chemoradiotherapy followed by resection were studied. Treatment-induced response at the primary site was evaluated by TRG and by a method whereby patients were classified as having no residual cancer, minimal residual disease (MRD) or as non-responders.
RESULTS: Between 2000 and 2007, 108 patients underwent resection. Disease-related survival decreased with increasing TRG in node-negative (N0) patients (P < 0.001), whereas in node-positive (N+) patients it was poor irrespective of TRG (P = 0.241). For N0 disease, 3-year survival in patients with MRD (58 (95 per cent confidence interval 26 to 80) per cent) was intermediate between that in patients with no residual cancer (85 (70 to 93) per cent) and non-responders (28 (4 to 59) per cent). Worst prognosis was for N+ disease (21 (9 to 36) per cent).
CONCLUSION: Node category should be considered when evaluating response to induction therapy in oesophageal or cardia cancer. A new classification based on size of residual foci and node category seems promising.
Prognostic significance of the Mandard TRG classification after induction therapy in carcinoma of the oesophagus and cardia
PubMed - VEDI IL LINK
Zanoni A, Verlato G, Minicozzi A, Tomezzoli A, Giacopuzzi S, Di Cosmo M, Franceschetti I, Saladino E, De Manzoni G.
Chir Ital. 2009 Jul-Aug;61(4):419-25.
Abstract
Mandard’s tumor regression grade (TRG) is widely used to evaluate the pathological response to induction therapy with concurrent chemoradiotherapy in cancer of the oesophagus or gastro-oesophageal junction. The aim of this study was to evaluate the prognostic significance and clinical applicability of TRG. From 2000 to 2007, 108 patients with squamous cell carcinoma of the oesophagus (57 cases) or Siewert type I and II adenocarcinoma of the cardia (51 cases) were treated with induction chemoradiotherapy followed by surgery in the 1st Division of General Surgery of the University of Verona. The treatment was identical for all patients and consisted of cisplatin, 5 FU and docetaxel together with 50 Gy of concurrent radiotherapy. The treatment-induced response was evaluated by TRG. Fifty-one, 24, 17, 9 and 7 patients were classified, respectively, as TRG1, 2, 3 4 and 5. Fifty-two patients died of the disease. Disease-related survival decreased with the increase in TRG class in node-negative patients (p < 0.001), while in N+ patients it was poor, irrespective of TRG class (p = 0.241). Mandard TRG is therefore useful for staging patients undergoing preoperative chemoradiotherapy, because it displays high prognostic significance. In our study, however, N was the main prognostic factor and for this reason it is mandatory to consider nodal status along with TRG. Moreover, among N negative patients, the prognosis of each different TRG class is statistically different and for this reason different TRG classes cannot be grouped together.
Reintervention after Heller Myotomy for Achalasia: Is It Inevitable?
PubMed - VEDI IL LINK
Raja S, Schraufnagel DP, Blackstone EH, Murthy SC, Thota PN, Thuita L, Lopez R, Gabbard SL, Ray MN, Wadhwa N, Sanaka M, Zanoni A, Rice TW.
Ann Thorac Surg. 2018 Nov 10. pii: S0003-4975(18)31629-1. doi: 10.1016
Abstract
BACKGROUND
Few studies of reintervention after Heller myotomy for achalasia set patients’ expectations, assist therapeutic decision-making, and direct follow-up. Therefore, we investigated the frequency and type of symptoms and reinterventions post-myotomy based on achalasia type.
METHODS
From 1/2006-3/2013, 248 patients who had preoperative high-resolution manometry and a timed barium esophagram (TBE) underwent Heller myotomy, 62 (25%) for type I, 162 (65%) type II, and 24 (10%) type III achalasia. Postoperative surveillance, including TBE, was performed at 8 weeks, then annually. Median follow-up was 36 months. Endpoints were all symptom types and modes of reintervention, endoscopic or surgical. Reintervention was based on both symptoms and objective TBE measurements.
RESULTS
Eventually most patients (169/218; 69%) developed at least 1 symptom post-myotomy. Fifty patients underwent 85 reinterventions, 41 endoscopic only, 4 surgical only, and 5 both. Five-year freedom from reintervention was 62% for type I, 74% type II, and 87% type III, most occurring within 6 months, although later in type III. At 5 years, number of reinterventions per 100 patients was 72 for type I, 51 for type II, and 13 for type III. After each reintervention, there was approximately a 50% chance of another within 2 years.
CONCLUSIONS
Patients’ expectations when undergoing Heller myotomy for achalasia must be that symptoms will only be palliated, and those who have worse esophageal function-achalasia type I-may require 1 or more postoperative reinterventions. Thus, we recommend that patients with achalasia have lifelong annual surveillance after Heller myotomy that includes a TBE.


Dott. Andrea Zanoni
dott.andreazanoni@gmail.com
Ospedale S. Maria del Carmine
Corso Verona, 4 - 38068 Rovereto - Trento
Privacy Policy
